Detailed data sheds new light on racial disparities in COVID-19 deaths
Published: Jun 25, 2020
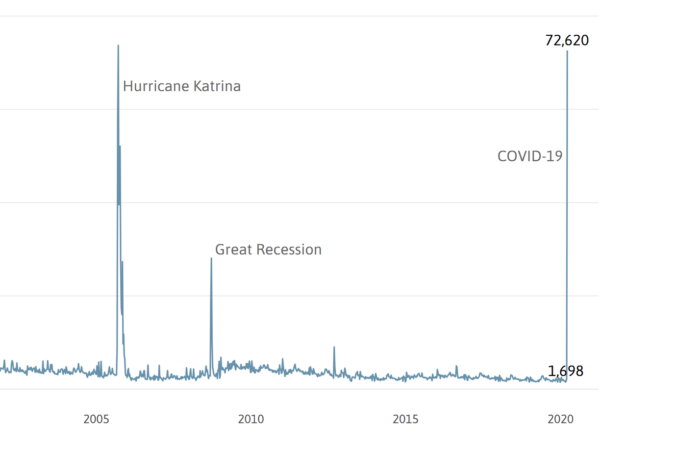
Despite a daily deluge of COVID stats, the available data still doesn’t tell us nearly enough about who and where COVID impacts are greatest and how we can mitigate them. Recent efforts to dig deeply into sporadically available but detailed data reveal two important preliminary findings:
- “Long-term care facilities” such as nursing homes and assisted living facilities are experiencing high rates of COVID deaths relative to their small resident populations.
- Nonetheless, the majority of deaths are taking place among residents not living in long-term care (LTC) facilities, and among this population, death rates for African Americans are higher than previously thought.
These two major trends could provide significant guidance about COVID mitigation activities as new waves of the pandemic emerge, but the available data on COVID cases and deaths is insufficiently broken down by race and group quarters on an ongoing basis. Cobbling together national studies, limited data released by Louisiana on nursing home deaths, and detailed data acquired from the Orleans Parish Coroner’s office, here’s what we know from the data so far:
Nursing homes and other long-term care (LTC) facilities represent a notable share of COVID deaths
Nursing homes and other LTC facilities account for a large number of COVID-19 deaths nationally and locally. The Centers for Disease Control and Prevention (CDC) estimates that 0.6 percent of the U.S. population lives in nursing homes or assisted living facilities, yet they account for 42 percent of all COVID-19 deathsi. Among 47 states reporting long-term care facility deaths, one study estimates there have been approximately 1,929 COVID-19 deaths per every 100,000 nursing home residents 65 years and olderii.
Louisiana does not publish COVID death data for assisted living or other LTC care facilities, but does provide weekly data on COVID deaths in nursing homes. The COVID death rate in Louisiana nursing homes has been quite high at 5,350 per 100,000 residents as of June 15th.
COVID-19 mortality rate in nursing homes per 100,000 residents
Rate per 100,000 nursing home residents
In St. John the Baptist Parish, which has experienced the highest COVID death rate in the state, over half of the deaths took place in two nursing homes. The death rate in St. John nursing homes is a stunning 26,381 per 100,000 as of June 15th, compared to 94 per 100,000 in St. John’s non-nursing home population.
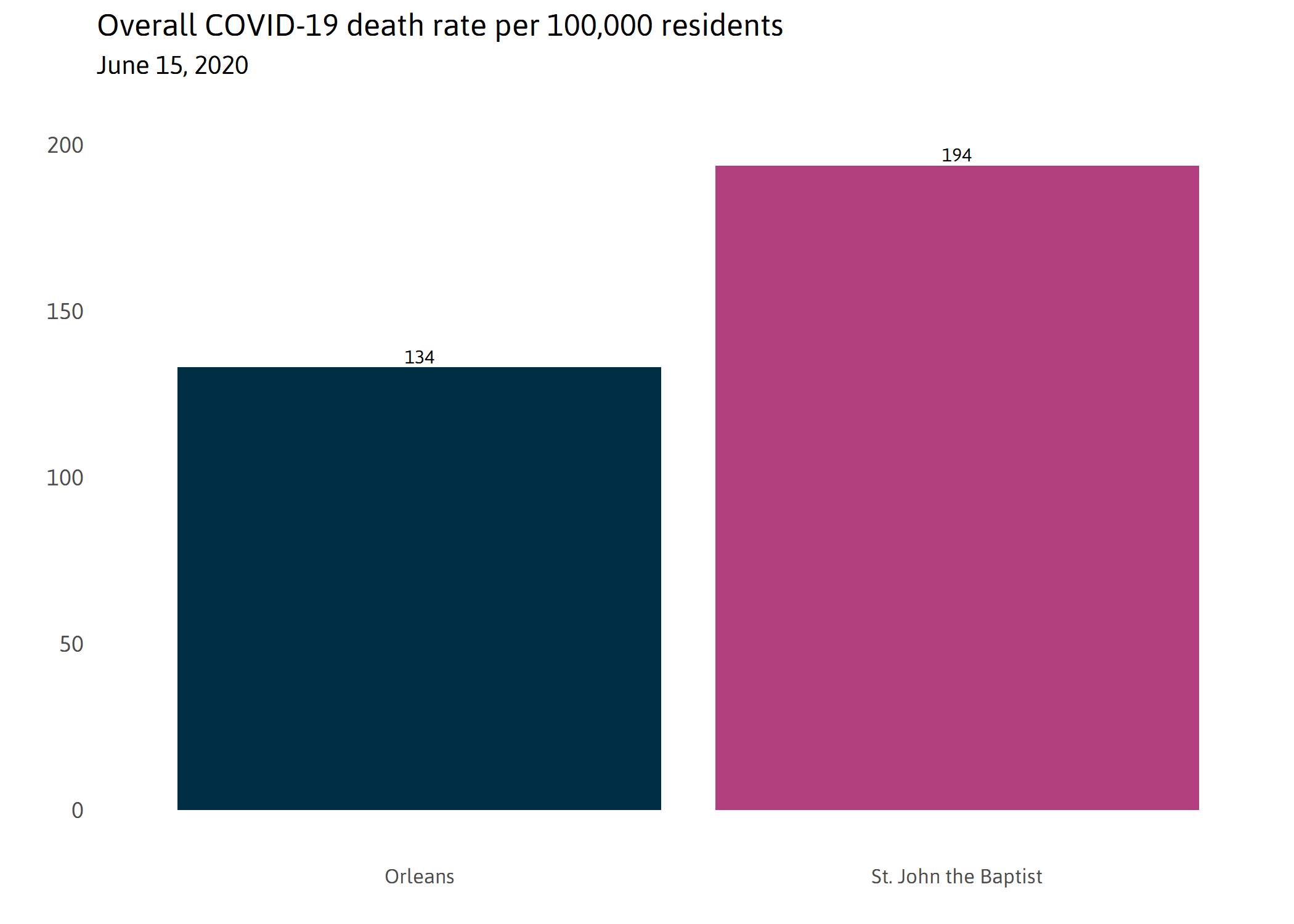
Looking at overall death rates by parish, St. John the Baptist seems to have consistently had the highest COVID death rate in Louisiana since April 1st with Orleans Parish a distant 2nd. As of June 15th, St. John has experienced 194 deaths per 100,000 and Orleans has experienced 134 per 100,000. But disaggregating death rates in nursing homes facilities from the non-nursing home public yields very different conclusions. For example, once we factor out deaths in nursing homes, we find that Orleans has a higher death rate at 107 per 100,000 than St. John the Baptist at 94 per 100,000 among the non-nursing home population.
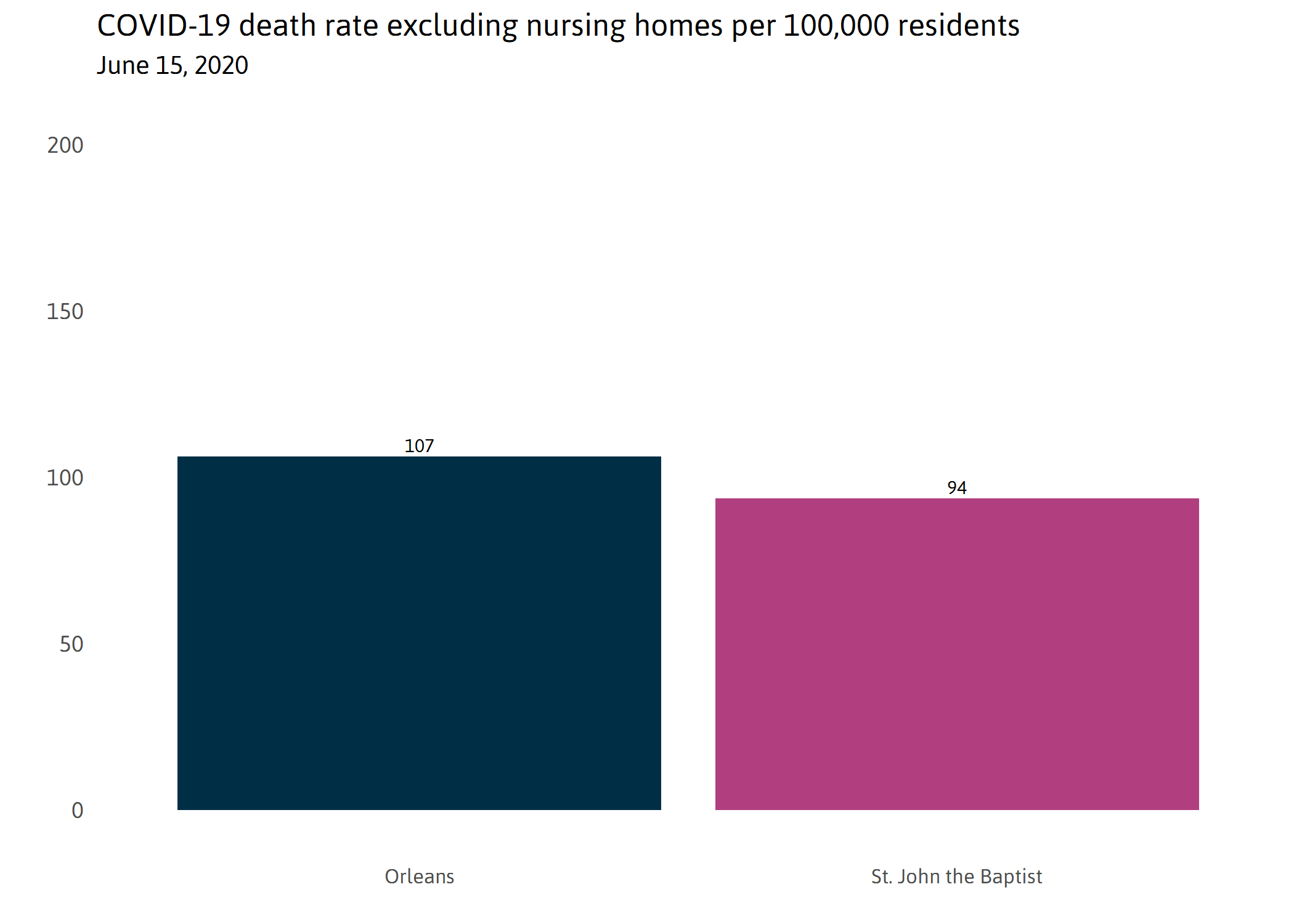
In New Orleans, 0.4 percent of residents live in nursing homes, yet they account for 20 percent of all COVID-19 deaths. The death rate in the New Orleans nursing home population is 6,714 per 100,000 compared to 107 deaths for every 100,000 non-nursing home New Orleans residents.iii
When you exclude LTC deaths, racial disparities in COVID deaths are even higher than first thought in New Orleans
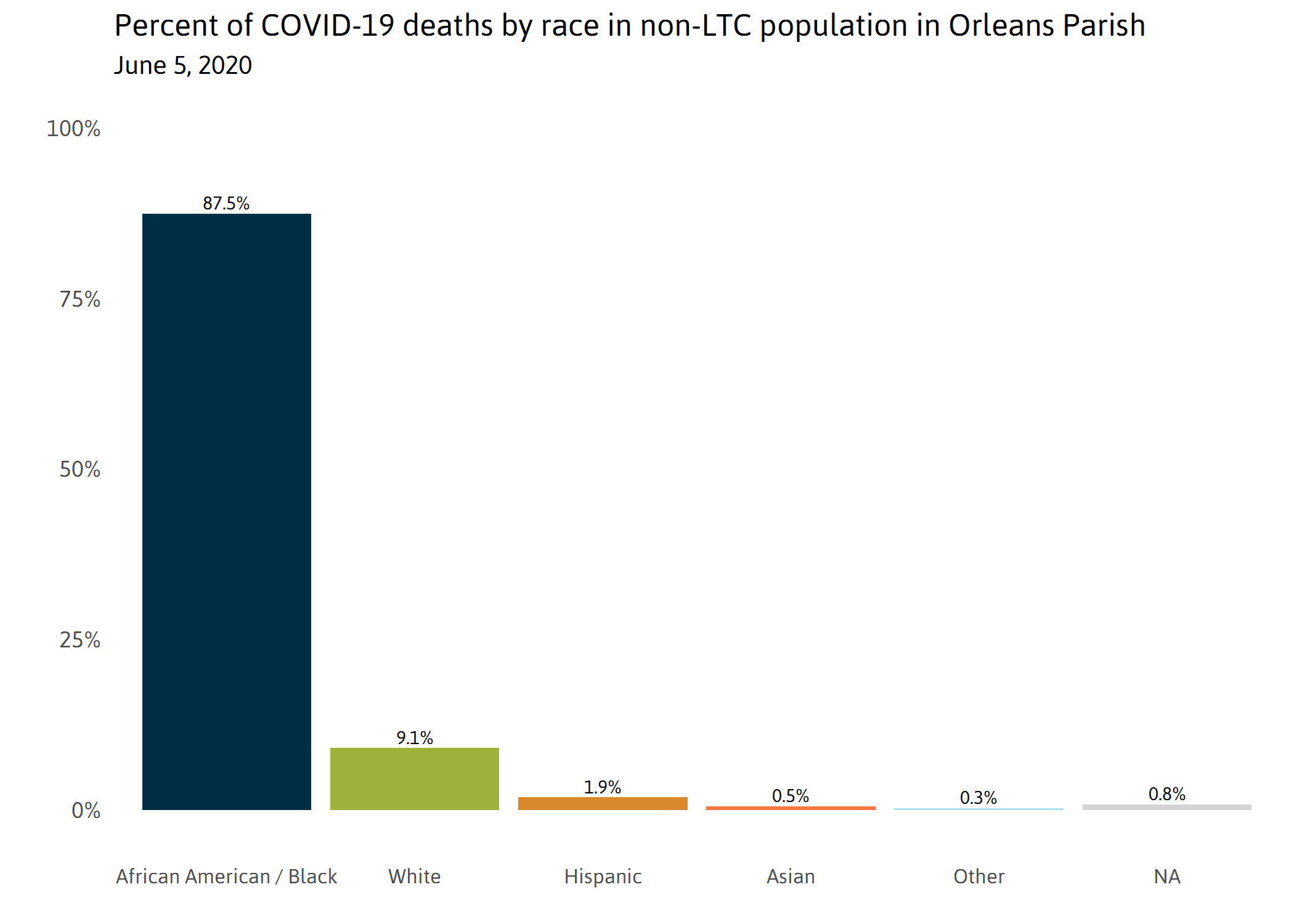
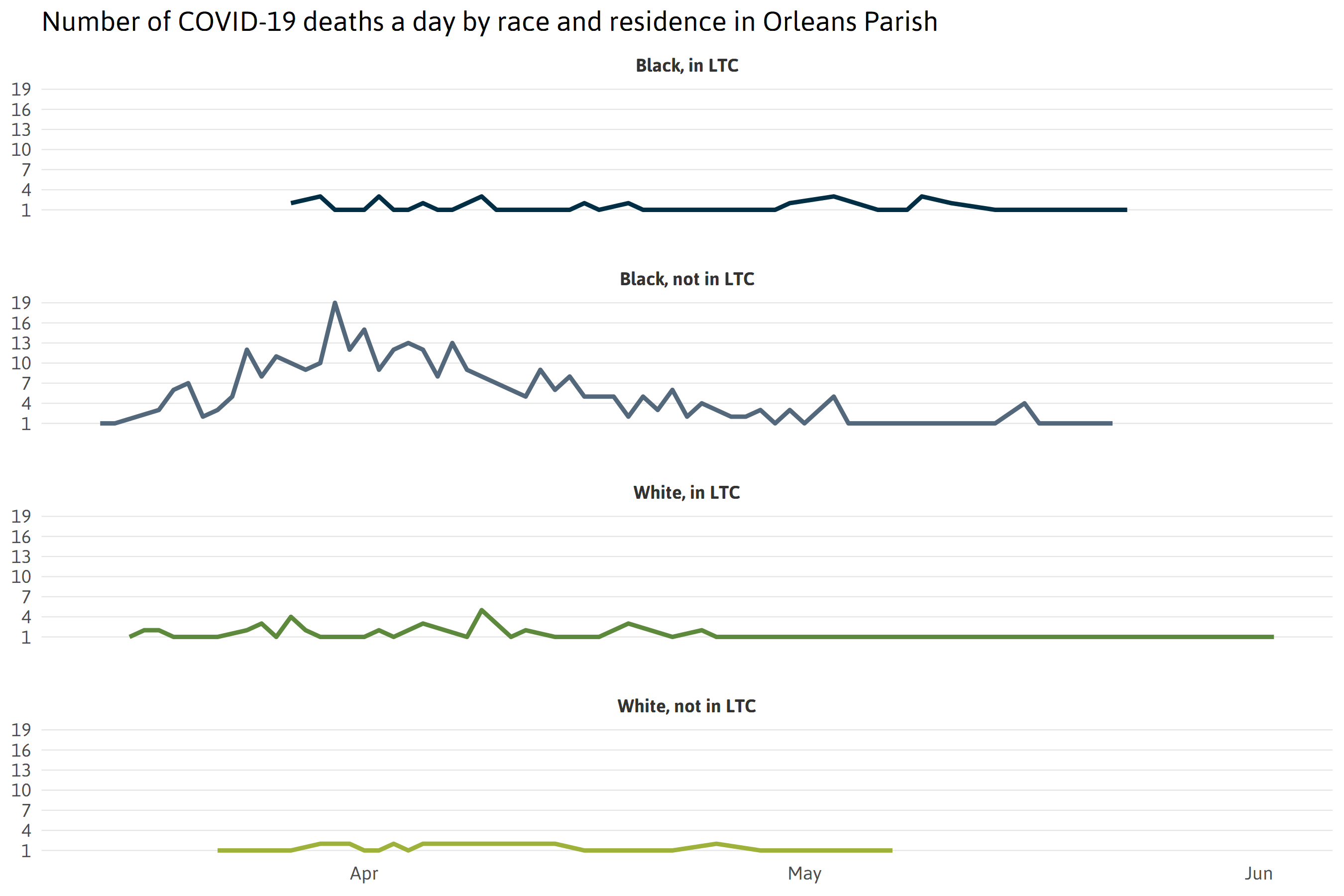
According to the Coroner’s data, as of June 5th black residents accounted for 77 percent of the 492 COVID-19 deaths in Orleans Parish, with white residents accounting for less than 20 percent (the population of Orleans Parish is 60 percent black and 35 percent white). While LTC deaths represent a notable share of those deaths in New Orleans (and elsewhere), the vast majority – nearly 80 percent – of COVID deaths were among New Orleanians who do not live in LTC facilities. After factoring out LTC deaths, racial disparities in New Orleans are far larger than previously known. Black New Orleanians account for nearly 88 percent of all non-LTC deaths, whereas white New Orleanians account for a much lower 9 percent.

Notes: A person who died from COVID-19 was designated as “non-LTC population” if their home address recorded in the Orleans Parish Coroner report was residential and not identified as a group home facility.
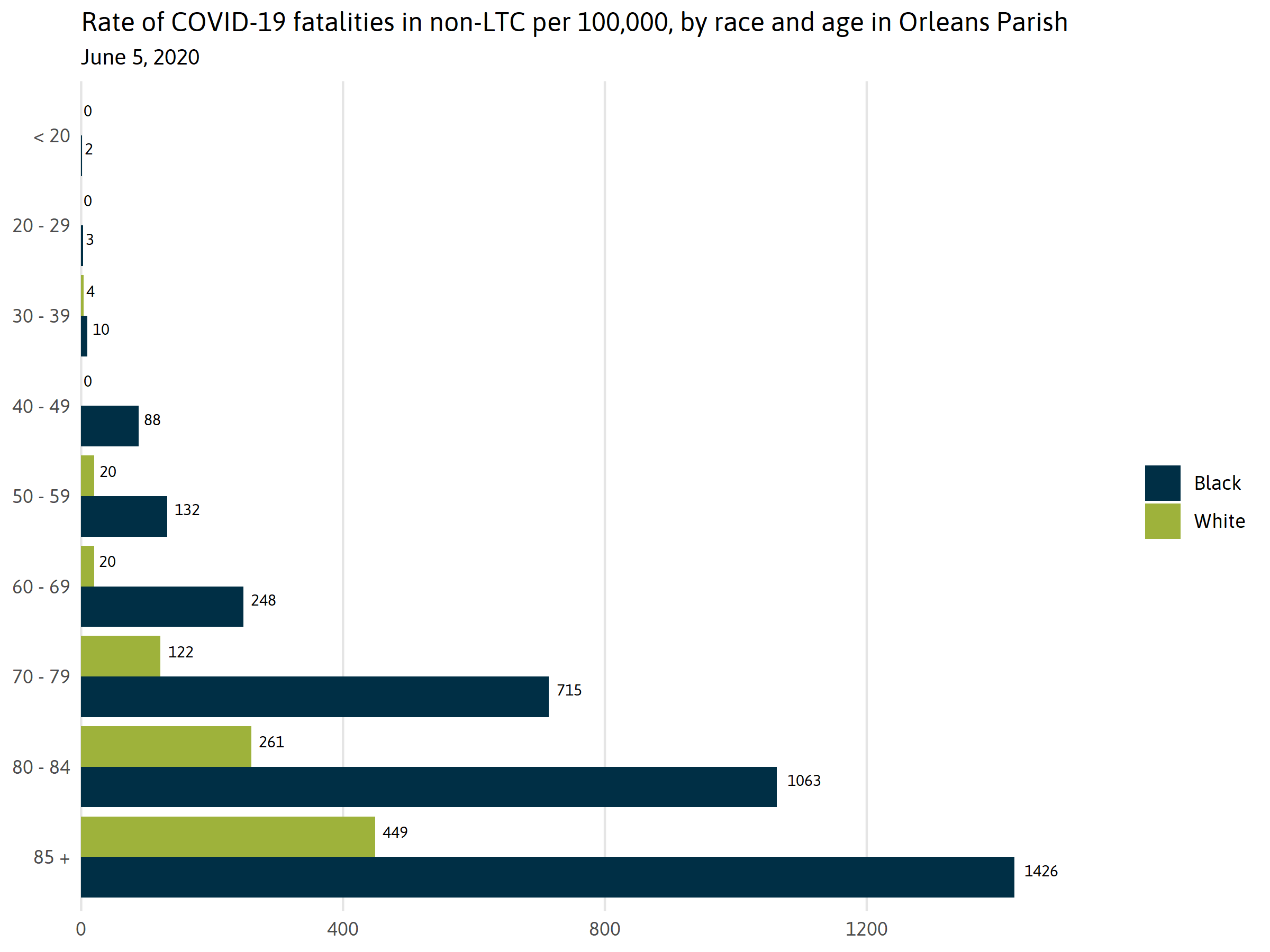
At every age, black New Orleanians are dying at higher rates than white New Orleanians in the non-LTC population.
- For all age groups 50 years or older, black people are dying at three to twelve times greater rates than white people.
- For every 100,000 black New Orleanians 85 years and older, there have been 1,426 COVID-19 deaths, compared to only 449 deaths for every 100,000 white New Orleanians that same age.
Why are death rates so much higher for African Americans?
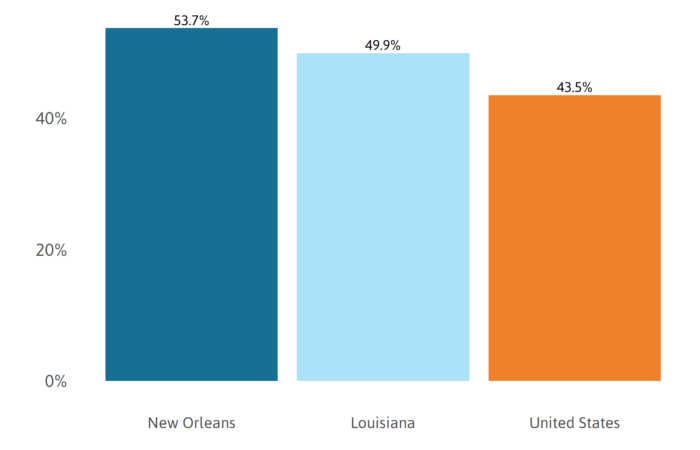
Emerging research suggests that racial disparities in COVID-19 deaths are multi-factorialiv. A larger portion of African Americans are employed in frontline essential positions where they are exposed to COVID on a daily basis. Across the New Orleans metro area, workers of color are overrepresented in essential retail (56 percent), transportation and trade (50 percent), and health care and social assistance (49 percent).v
African Americans are more likely to live in multi-generational homes. In Orleans Parish in 2018, there were over seven times more multi-generational black homes than there were whitevi. The CDC recommends “If your household includes people in these [at risk] groups, then all family members should act as if they, themselves, are at higher risk” and “stay at home as much as possible.“vii However, many essential workers, especially those who earn lower wages may not have the luxury of staying home without losing their job. Thus, they may be exposed to COVID, bring it home to vulnerable older adults, but struggle to isolate themselves from their family members if, for example, their homes have only one bathroom that all family members must share.
Indeed, black New Orleanians are much more likely to experience multiple COVID-19 deaths in the same family. According to the Coroner’s records as of June 5th, 36 individuals who have died of COVID-19 in New Orleans lived in a household where at least one other person died from COVID-19, 35 of whom were African American. Many of those victims were married couples, siblings, or adult children and their elderly parents as identified through public obituaries and news articles.
COVID infections and deaths in black and white communities are interconnected.
There is no doubt that the lives of black and white folks intersect frequently in New Orleans and many localities across Louisiana and the nation. For example, many nursing home aides provide hands on care to nursing home residents and, as described above, infected nursing home residents can easily infect aides who then bring the infection home. If the aide happens to live in a smaller home with limited ability to isolate sick family members, then the infection risks associated with the workplace are more easily transferred to the home. Because black nursing home aides need not only support black nursing home residents, nor are white aides restricted to white residents, the interconnection between black and white communities means that when infection rates rise in white communities, we might expect them to rise in black communities, and vice versa.
Indeed, COVID deaths rates for both blacks and whites in New Orleans greatly exceed their peers nationally. Specifically, the death rate among black New Orleanians is 164 per 100,000 (compared to 61.6 per 100,000 for blacks nationally), and the death rate for white New Orleanians is also substantially higher at 73 per 100,000 (compared to 26.2 per 100,000 for whites nationally) as of June 9th. Our analysis of death rates by race across the 43 states reporting deaths by race reveals that states with higher than average black death rates have higher than average white death rates as well.viii
Black and white COVID-19 mortality rate per 100,000 residents
June 9, 2020
Implications for COVID mitigation policies and practices
Though much of the data in this brief focuses on New Orleans, the trends are largely consistent with national studies. Protecting our communities when new waves of the pandemic emerge will remain a substantial challenge. The ability to safely social distance is a privilege that comes with telecommuting, paid sick leave, and safer working conditionsix. Limited access to transportation, smaller housing units, and the effects of racism in health care provisions are some of the daily realities to be considered when planning the next phase of COVID mitigation.x Decisionmakers should prioritize vulnerable low-income minority neighborhoods for mobile testing. And all infected individuals should be offered “supported isolation” away from family members with comprehensive case management that identifies and meets needs such as lost wages, childcare, and elder care services. Essential public facing jobs, such as schools, childcare centers, and nursing homes, alongside professionals in healthcare settings and first responders, should receive priority for PPE and testing.
Nursing homes and other LTC facilities are especially vulnerable to COVID-19 because their residents are older with high rates of chronic conditions. Nursing home residents who test positive for COVID but do not require hospitalization should not return to their facility but instead should be provided with “supported isolation” services elsewhere. Importantly, nursing homes are not isolated but are connected to their surrounding communities through workers and visiting friends and family. Even under the strictest “lock down” scenario, essential staff still come and go between shifts. Additionally, staff often do not have paid sick leave, disincentivizing them to stay home when experiencing symptoms.xi In this way, nursing homes can be sources of outbreak that affect the larger community.xii
To fully understand how outbreaks in nursing homes may spread to the larger community, more data is needed on cases and deaths among nursing home workers. Beyond nursing homes, all long-term care facilities should be legally mandated to report COVID cases and deaths among residents and workers.xiii In addition, data on contact tracing will be critical going forward to determine where and how new outbreaks emerge. As the city and state begin to allow for larger gatherings such as church services, contact tracing data will be essential for discerning which settings and activities are most likely to act as “super spreaders.” Contact tracing data should also be linked to coroner’s records to determine which settings and activities are most fatal.
Other institutionalized populations such as prisons, jails, and group homes must also be scrutinized. These institutions often disproportionately impact the same communities that are at highest risk of contracting COVID, and present major structural barriers to disease preventionxiv. Indeed, as of June 17th nationwide, correction facilities represented the five largest known coronavirus clusters, and COVID prison deaths have risen 73 percent since mid-May.xv Although no deaths have yet been reported in Orleans Justice Center (formerly named Orleans Parish Prison), the state has begun testing all inmates since a prison warden tested positive for the virus.xvi There is an urgent need to assess the safety of all institutionalized populations during this outbreak. Failing to do so could have major ramifications for the city, state, and nation as a whole.
Methodology
The Data Center obtained data from the Orleans Parish Coroner’s Office on every death in the parish until June 5th with COVID-19 listed as the cause of death. Among other information, the data included the race, age, sex, home address, location and time of death for nearly each person. After a laborious cleaning process, this data was compared against a list of licensed providers in the state to determine if a person was living at home or in a group home facility at the time of their death. Matching addresses of those who did die in facilities shed light on the type and name of facilities where outbreaks were occurring. There were too few people classified as “Asian”, “Hispanic”, or “Other” among those reported to have died by COVID-19 in Orleans Parish at this time to reliably interpret findings, so the majority of this analysis focuses only on those whose race was classified as “White” or “African American/Black”.
There are several kinds of Long-Term Care facilities. As of June 5, 2020, the Orleans Parish Coroner’s office reported deaths in long-term care facilities as follows.
| Residence | Number of deaths | Percent of total deaths |
|---|---|---|
| Private residential address | 375 | 76.2% |
| Nursing home | 92 | 18.7% |
| Adult Residential Care | 18 | 3.6% |
| Behavioral Health Service | 4 | .8% |
| Intermediate Care Facility/Developmentally Delayed | 2 | .4% |
| Home and Community Based Services | 1 | .2% |
The Louisiana Department of Health provides these cautions regarding nursing home COVID rate calculations. “The census counts for many facilities have decreased over time. Some nursing homes are actively accepting COVID patients from other facilities; case counts for these nursing homes may include individuals diagnosed at another facility. Currently, all deaths in individuals with COVID positive lab results are being counted, this may include individuals with pre-existing conditions or individuals ultimately determined to have another cause of death.” In addition, not all nursing home residents who have died since the pandemic outbreak were tested for COVID, thus, the total number of COVID deaths in nursing homes may be larger than reported.
Footnotes and Sources
iii http://ldh.la.gov/assets/oph/Coronavirus/NursingHomes/NHReport061520.pdf.
Notes: 14 of the 492 total deaths were excluded from this analysis because they were residents of a facility other than a nursing home that does not provide resident population. Adult residential care facilities are similar to nursing homes but not legally required to report COVID-19 cases, deaths, or an updated count of residents.iv Price-Haywood, E. G., Burton, J., Fort, D., & Seoane, L. (2020). Hospitalization and Mortality among Black Patients and White Patients with Covid-19. New England Journal of Medicine.
v https://www.datacenterresearch.org/reports_analysis/who-are-the-essential-workers-keeping-the-new-orleans-region-going/
vi The Data Center analysis of American Community Survey 2018.
viii https://www.apmresearchlab.org/covid/deaths-by-race#reporting
Note: As of 6/9 there were 6 states not reporting deaths by race, and Texas’s death by race data is public but considered “poor quality”.
ix Yancy, C. W. (2020). COVID-19 and African Americans. Jama.
x https://rubixls.com/2020/04/01/health-data-in-the-covid-19-crisis-how-racial-equity-is-widening-for-patients-to-gain-access-to-treatment/
xi Barnett, M. L., & Grabowski, D. C. (2020, March). Nursing homes are ground zero for COVID-19 pandemic. In JAMA Health Forum (Vol. 1, No. 3, pp. e200369-e200369). American Medical Association.
xiv Wurcel, A. G., Dauria, E., Zaller, N., Nijhawan, A., Beckwith, C., Nowotny, K., & Brinkley-Rubinstein, L. (2020). Spotlight on jails: COVID-19 mitigation policies needed now. Clinical Infectious Diseases.
xv https://www.nytimes.com/2020/06/16/us/coronavirus-inmates-prisons-jails.html?campaign_id=9&emc=edit_nn_20200616&instance_id=19429&nl=the-morning®i_id=78001017&segment_id=31015&te=1&user_id=89b05474f28af4c52697afe4e3d1f71e